
Have you considered how your body might react to the same foods as your neighbours? The idea of personalised nutrition challenges the old belief that diet advice should be the same for everyone.
For almost ten years, scientists have noticed that precision nutrition could fill big gaps in food science by looking at how people react to diets. What we eat has a big impact on worldwide health problems like obesity, type 2 diabetes, and heart disease. However, new studies indicate that these illnesses develop through numerous complex pathways that differ significantly from one individual to another. This phenomenon explains why programmes like the NIH Nutrition for Precision Health project and the All of Us Nutrition for Precision Health plan are getting more attention.
Our gut microbiota influences about 10% of the differences between individuals we see after they eat. A study with 800 people backed this up. The study developed customised models to predict glucose levels based on blood markers, eating habits, lifestyle factors, and gut bacteria. Furthermore, scientists found that the amount of certain gut bacteria at the start can predict how well people will lose weight on low-calorie diets.
In this article, we’ll look into why old nutrition models don’t work well, refer to the science behind precise nutrition, and see how experts create and give personal diet plans in 2025.
Why Old Nutrition Models Don’t Work in 2025
Traditional nutrition models have long worked on the idea that general dietary advice works for everyone. However, new research shows big problems with this approach, especially since we’ve learnt more about how different people’s bodies work.
Problems with One-Size-Fits-All Diet Guidelines
The strongest proof against standard nutrition advice comes from studies that show significant differences in how people react to the same meals. Research shows that insulin, blood sugar, and blood fat responses to the same foods can vary a lot even between identical twins. For example, one twin may handle carbs well but struggle with fats, while the other is the opposite. This biological variety challenges the foundation of universal diet guidelines.
Despite what many think, genetics has a small impact on how our bodies react to food. Therefore, simple DNA tests that claim to identify “the perfect diet for your genes” are ineffective and can mislead individuals. Furthermore, diets that tell you to eat a set number of calories or specific amounts of protein, carbs, and fats are too simple. They don’t take into account that each person’s body functions differently.
Official guidelines tell us to eat various healthy foods. But these guidelines still assume that most people need the same nutrients. In reality, there are numerous ways to combine different foods. This approach allows each person to receive the exact nutrients their body needs.
Inconsistencies in Nutrient-Disease Associations
While observational data has indicated strong links between various diet factors and chronic disease risk, randomised controlled trials (RCTs) set up to test these connections often show no effect. This difference has led to uncertainty among healthcare pros and the public alike.
These conflicting results bring up big questions about how we decide if evidence warrants starting large-scale clinical studies. The issue grows trickier when we think about how nutrition interventions have many parts that interact, with lots of variation in what we measure as outcomes.
Additionally, studies show that 43% of people have trouble finding reliable information about healthy eating. The most confusing sources of diet advice are the media (76%) and experts (61%). This contradictory nutrition information (CNI) becomes tricky on social media, which now swarms with false health claims.
Hurdles in Applying Research to Public Health
Diet studies in clinical settings face many obstacles that restrict their real-world use. These include the intricate nature of diet interventions, overlapping diet components, varied eating habits, and different food cultures. Therefore, transforming nutrition research into effective public health plans continues to be a challenging task.
In real-world studies, poor compliance (30-50%) and high dropout rates (20-49%) create major obstacles for long-term studies. Furthermore, it’s often impossible to blind participants and carers in diet studies, which can lead to bias.
Food and drink companies have a giant impact on dietary guidelines, sometimes resulting in vague or questionable recommendations. For example, even though science supports eating less red meat and ultra-processed foods, pressure from the industry has kept such advice out of official guidelines.
Public health nutrition depends on turning research into real-world practices and policies. It ensures that interventions based on evidence improve nutrition-related behaviours and health outcomes. Above all, researchers and practitioners must work together to create interventions that can be used in real-life settings.
The Scientific Foundation of Precision Nutrition
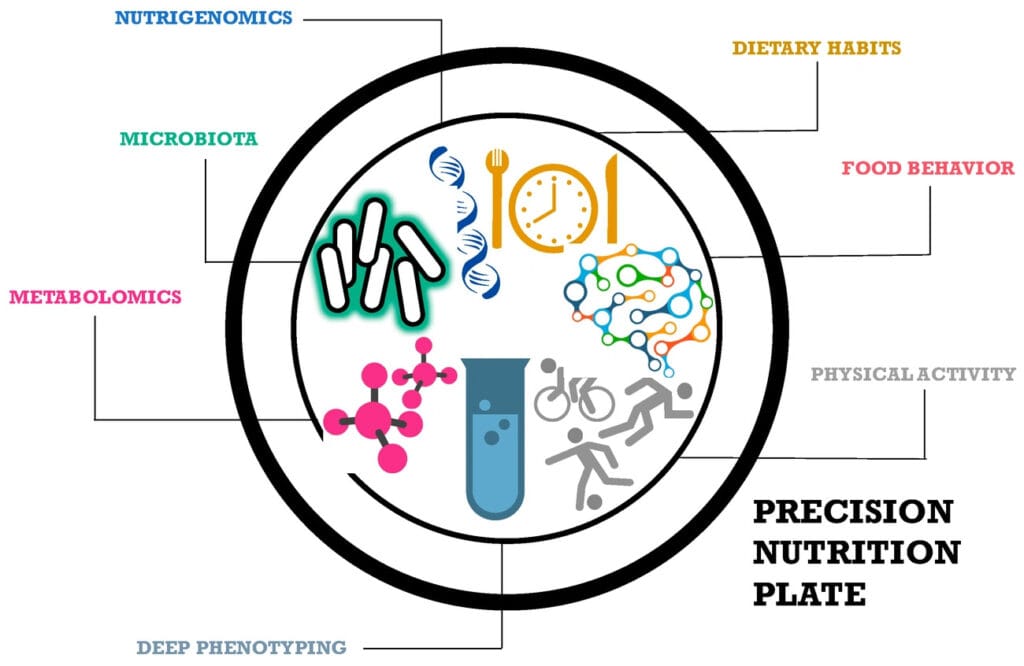
Image Source: MDPI
Precision nutrition stands on three connected biological foundations that explain why people react to the same diets. These core elements give scientific backing to move past standard dietary advice that treats everyone the same.
Gene Differences and How We Use Nutrients
The human genome has well over 3 million single DNA letter changes compared to the standard genome, with about 1% of a person’s genes differing from this standard sequence. These genetic changes have a big impact on how we handle and use nutrients. In fact, common changes in genes linked to nutrient use affect what nutrients each person needs, takes in, and uses.
For instance, alterations in the methylenetetrahydrofolate reductase (MTHFR) gene influence the metabolism of folate and are associated with heart disease and diabetes. People with the homozygous mutation (TT) in the MTHFR gene might need to eat more folate than recommended. In the same way, genetic differences in beta-carotene oxygenase 1 (BCMO1) can cause changes in plasma carotenoid levels, which could affect vitamin A levels in the body.
The Apolipoprotein E (ApoE) gene offers another key example. Its three forms—ApoE2, ApoE3, and ApoE4—have an essential role in moving cholesterol and breaking down fats. The ε4 type links to higher chances of heart and Alzheimer’s disease. Testing for these gene types can help create specific plans to prevent disease.
How Early-Life Food Affects Genes
What we eat in life can change how our genes work without changing the DNA itself. These changes create a kind of biological “memory” of past eating habits and can shape our health for life. The first years of life are when food is most likely to cause these gene changes.
A mother’s diet has a big impact on her baby’s epigenome in several ways:
- DNA methylation: Nutrients in one-carbon metabolism (folate, choline, betaine, methionine) work as methyl donors, while vitamins B12, B6, and B2 act as helpers
- Histone changes: What a mother eats affects histone methylation and acetylation, changing how easy it is to access genes
- MicroRNA control: Food choices shape microRNA levels, which control gene activity
Studies on the Dutch Famine group show that people exposed to famine before birth had, 60 years later, less DNA methylation of the imprinted IGF2 gene than their siblings who weren’t exposed. Later, researchers found that when mothers ate more omega-3 polyunsaturated fatty acids, their newborns showed signs of slower epigenetic ageing. In contrast, saturated fat had the opposite effect.
Gut Microbiome Diversity and How Diet Affects It
The gut microbiome, often called a “forgotten organ,” plays a key role in keeping the body balanced and healthy. The microbiome acts as a crucial go-between in breaking down, absorbing, and using the components of our diet.
Diet over long periods seems to have the biggest known effect on what kinds of bacteria live in our guts, more than any other outside factor. Research shows that people who eat lots of fibre and carbs tend to have more Prevotella bacteria. On the flip side, those who eat a typical “Western” diet with lots of protein and fat have more Bacteroides bacteria.
Scientists keep noticing that different people’s gut bacteria react to changes in diet. How much a person’s gut bacteria change depends on what their gut was like to start with. This includes things like how many different types of bacteria they have, how much of certain kinds of bacteria there are, and what those bacteria can do. This phenomenon is why the same diet can lead to different results in different people’s bodies.
New studies have identified two distinct bacterial groups in the gut microbiome: the positive Foundation Guild and the harmful Pathobiont Guild. The Foundation Guild breaks down dietary fibres and produces short-chain fatty acids that are crucial for gut health. When the Pathobiont Guild takes over the gut ecosystem, it can make diseases worse. The balance between these guilds plays a key role in determining how individuals respond to dietary changes within the nutrition for precision health framework.
How Precision Nutrition is Measured and Delivered

Image Source: MDPI
Turning scientific insights about precision nutrition into real-world uses calls for cutting-edge measuring tools and delivery methods. These gadgets help us spot individual differences that old-school approaches overlook.
Biomarkers of Food Intake and Nutritional Status
Nutritional biomarkers offer concrete measurements of what people eat and their nutritional health, going beyond the drawbacks of self-reported information. These biomarkers don’t suffer from memory errors or people trying to supply acceptable answers, unlike traditional ways of assessing diet. Biomarkers fall into several groups:
- Exposure biomarkers show what specific foods someone has eaten (for example, urine nitrogen levels point to protein intake)
- Effect biomarkers signal how the body responds to nutrients
- Health/disease biomarkers indicate overall health or the risk of certain diseases
Biomarkers differ in how they measure intake—from recovery biomarkers that quantify actual consumption to concentration biomarkers that correlate with intake but metabolism affects them. Currently, research efforts within the NIH Nutrition for Precision Health initiative aim to validate these biomarkers against regular food intake patterns.
Wearable Devices and Real-Time Nutrient Monitoring
Real-time monitoring has changed from idea to reality through wearable technology. Continuous glucose monitors (CGMs) have become popular even among healthy people who want to improve their metabolic responses. Market forecasts suggest the CGM market by itself will grow to $5.50 billion as prices drop and more people start using them.
Beyond glucose, cutting-edge wearable biosensors now have an impact on sweat analysis to spot various metabolites, including amino acids and vitamins, even when resting. These non-invasive techniques give crucial data to shape tailored nutritional plans without needing invasive blood samples.
AI-Powered Dietary Assessment Tools
Artificial intelligence is causing a revolution in dietary assessment through automated food image analysis. Deep learning models can now spot foods, gauge portion sizes, and figure out nutritional content with growing precision. In comparison studies, AI-based portion size estimation reached relative errors as low as 0.10% for calories and 0.09% for volume in controlled environments.
Image-assisted dietary assessment (IADA) systems have evolved from simple algorithms to complex AI frameworks capable of analysing multiple foods simultaneously. Field studies show one AI system had a Mean Absolute Percentage Error (MAPE) of 31.9% when estimating portion sizes. This beats trained dietitians, who had a MAPE of 40.1%.
These technologies work together in the All of Us Nutrition for Precision Health program. This creates new chances to gauge and provide custom nutritional advice.
Designing Personalized Dietary Interventions
Personalised nutrition plans are becoming more than just suggestions. They’re turning into detailed, doable strategies that fit each person’s unique traits. This approach shifts the focus from what might work for most people to what will work just for you.
What to Eat: From Nutrients to Dietary Patterns
Instead of just looking at single nutrients, precise nutrition plans now focus on whole eating patterns made to fit individual needs. Based on biological markers, the USDA’s dietary patterns provide flexible frameworks for customisation. These patterns include the Healthy U.S.-Style, Healthy Mediterranean-Style, and Healthy Vegetarian Dietary Patterns. Each one comes in 12 calorie levels to meet different needs.
Personalised nutrition plans often group people into specific diet types based on their physical traits. In one tailored nutrition program, people received custom breakfasts and lunches five days a week for nine weeks. These meals matched their personal diet type, which led to better health results.
How to Eat: Cooking Methods and Food Processing
How you cook food affects its nutrition and safety. Cooking at high temperatures can create harmful substances. These form when amino acids, creatines, and sugars react. For example:
- Temperature has the largest impact on heterocyclic amine (HCA) formation, with issues starting at 212°F (100°C)
- Cooking methods that use direct heat like frying and grilling, create more HCAs than indirect methods such as stewing or steaming
- A 90-gram chicken breast can have between 1,000 and 9,000 advanced glycation end products (AGEs) based on how it’s cooked
Cooking at lower temperatures and using methods that involve liquids can cut AGE production by half, which can bring down plasma AGE levels by 30% in just a month.
When to Eat: Time-Restricted Feeding and Chrononutrition
Chrononutrition, which matches food intake with body clocks, is key to precision nutrition. Time-restricted eating (TRE) limits food to a 4- to 10-hour period during the day’s active phase. Studies show TRE leads to an average 3% weight loss and less body fat even without cutting calories.
Currently, most adults eat over a 12–15-hour span, with more than half eating for over 15 hours each day. TRE fixes this by matching eating times to natural body rhythms. The upside comes from better alignment of body clocks—syncing the main clock in the brain with other clocks throughout the body.
TRE has a positive impact on metabolism even without weight loss, hinting at an inherent effect that aligns eating patterns with the body’s natural rhythms. Health benefits persist even when people follow TRE during weekdays and eat freely on weekends.
Bringing Precision Nutrition to Everyone
Image Source: Redress Compliance
To spread the advantages of precision nutrition from individual treatments to larger groups, it’s key to implement it through existing healthcare systems. Currently, bringing personalised approaches to mainstream healthcare offers both possibilities and hurdles.
How Primary Healthcare Can Help with Personalized Diet Plans
Primary care doctors play a key role in giving tailored nutrition advice. Patients who discuss food with their doctors tend to lose more weight. They also face a lower chance of getting diabetes and heart problems. Yet many doctors find it difficult to discuss nutrition. They have little time during visits, food guidelines keep changing, and talking about diet can be emotional.
The Food4Me Study, the biggest trial of its kind, looked at how well personalised nutrition worked. It indicated that custom food advice pushes people to eat healthier much more than standard tips. This evidence supports the increased use of personalised nutrition in primary care.
AI Decision Support Systems for Clinicians
AI tools are changing how doctors give diet advice. Researchers at the University of Texas created “Nutri,” an AI tool that works with health records to personalise nutrition talks. This system shows patient diet info to doctors, helps set goals, keeps track of progress between visits, and even writes draft notes to cut down on paperwork.
AI health decision support systems provide doctors complete information from health records, exercise data, and gut bacteria profiles to make custom recommendations. By 2026, AI use in healthcare will save about $150 billion in the United States.
Integration with NIH Nutrition for Precision Health Study
The NIH Common Fund’s Nutrition for Precision Health program stands as the largest study of its kind in precision nutrition. This project plans to sign up 10,000 people from different backgrounds to create formulas that predict how each person reacts to certain foods and eating habits.
This study builds on the framework of the All of Us Research Program. It looks at how diet, genes, proteins, gut bacteria, metabolism, and other factors in a person’s life work together. People who join provide samples of their blood, spit, and poop. They also eat test meals that help scientists understand how each person’s body handles food.
Conclusion
Precision nutrition has a profound influence on how we grasp dietary science. This article looked at why the standard one-size-fits-all method doesn’t work for everyone’s unique biology. The facts show that even identical twins react very differently to the same meals.
Our genes, their expression, and the bacteria in our gut all contribute to these individual food responses. These biological basics give us good reasons to move past general food rules and focus on tailored approaches. As a result, today’s precision nutrition uses advanced tools—biomarkers, wearables, and AI-powered systems—to capture individual differences that old methods can’t see.
Tailored dietary plans now go beyond basic nutrient advice to include full eating patterns, cooking techniques, and meal schedules. Eating within set hours, in particular, has an impact on health by matching food intake with natural body rhythms even without changes in calorie consumption.
Bringing precision nutrition into regular doctor visits presents a big chance. AI tools help doctors give personalised advice during check-ups, while large projects, like the NIH Nutrition for Precision Health study, collect key data from many different groups to improve prediction methods even more.
Precision undoubtedly shapes the future of nutrition. Instead of wondering which foods are “healthy” for everyone, we now ask a better question: “Which foods are good for you?” This change in thinking doesn’t just lead to better diet advice. It also helps to better prevent and manage long-term illnesses. After all, custom-made nutrition backs up what studies keep showing—the diet that works best for you might not be ideal for someone else.
FAQs
Q1. What is precision nutrition, and how does it differ from traditional dietary advice?
Precision nutrition tailors diet plans to each person’s unique genetic makeup, gut microbiome, and metabolic responses to food. This approach stands apart from standard dietary guidelines that apply to everyone. It recognises that people react to the same foods and adjusts recommendations to suit individual needs.
Q2. How do genetic variations have an impact on our nutritional needs?
Genetic variations can shape how our bodies process and use nutrients. Take, for instance, genes linked to folate metabolism or vitamin A conversion. Differences in these genes can affect how much of these nutrients a person needs. Knowing these genetic distinctions allows us to create more targeted nutrition plans.
Q3. What role does the gut microbiome play in precision nutrition?
The gut microbiome has a significant impact on how our bodies digest and absorb nutrients from food. Different people have different gut bacteria compositions, which affect their responses to various diets. Precision nutrition considers each person’s unique microbiome profile when creating dietary plans.
Q4. What is the role of wearable devices in precision nutrition?
Wearable devices, like continuous glucose monitors, now track metabolic responses to food in real time. These devices supply useful data on how a person’s body reacts to different meals. Such information allows for more customised and individualised dietary advice.
Q5. Can precision nutrition help in managing chronic diseases?
Precision nutrition shows a lot of promise to help manage long-term health problems. This approach customises diet plans to match a person’s specific biology. It has an impact on improving nutrient intake, keeping blood sugar in check, and lowering inflammation. These benefits might lead to better results for people dealing with health issues like diabetes, heart disease, and weight problems.
